Modern eating and lifestyle patterns are rough on the digestive system. Most people eat more processed food, less fiber, sleep poorly, stay stressed, and use antibiotics frequently. All of this disrupts the gut microbiome—the community of bacteria and microbes living in the intestines.
When the microbiome loses balance, digestion slows, inflammation rises, and the gut lining becomes more sensitive. This is what we mean by poor gut health. It is not a trendy phrase. It’s a measurable shift inside the body.
Poor gut health usually involves three things happening at the same time:
The issue isn’t that the gut is “dirty” or needs “detox.” That’s nonsense. The real problem is imbalance.
The body is trying to digest food and manage immune signals all day long. But when diet and routine keep stressing the system, the gut starts reacting. This reaction shows up as bloating, gas, constipation, or even mood and sleep changes. These symptoms aren’t random. They’re signals indicate the gut is struggling to maintain control.
This article focuses only on real biology and practical steps backed by research. No vague wellness slogans. No miracle cures. The goal is simple and clear: understand the symptoms, fix the causes, and restore balance naturally.
What Does the Gut Actually Do
The gut is not just where food goes. It’s a control center for digestion, immunity, and even mood. Understanding what it does makes it easier to see why poor gut health affects the whole body.
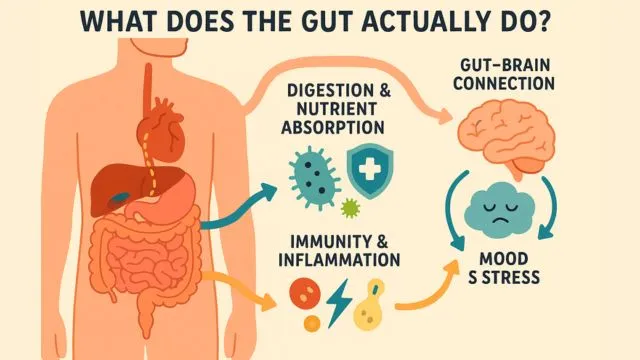
- 1. Digestion and Nutrient Absorption: The gut breaks down what you eat into forms your body can use. Food → nutrients → energy and cell repair. If digestion is slow or weak, you feel heavy, bloated, or tired. When nutrients don’t absorb well, even a “healthy diet” won’t feel like it’s helping. So when the gut struggles, the whole body feels low on fuel.
- 2. Microbiome and Immune System Defense: Inside the gut lives the microbiome—trillions of bacteria and microbes. Helpful bacteria protect the gut lining. They fight harmful microbes and reduce inflammation. About 70% of the immune system is located around the gut. If the microbiome gets disrupted, Inflammation increases, the body becomes more reactive, and the minor triggers start causing major discomfort.
- 3. Gut–Brain Connection (Why Stress Hits Your Stomach): The gut and brain communicate through the vagus nerve. Stress can slow digestion → bloating, tightness, nausea. Anxiety can speed digestion → loose stools, urgency. Gut bacteria also produce some neurotransmitters involved in mood. This is why stress shows up as stomach discomfort, and poor gut health can feel like low mood, irritability, or foggy thinking.
Note: Gut health influences mood and inflammation, but does not control everything. It’s correlation, not automatic causation. Fixing the gut supports balance; it’s not a cure-all.
Key Idea: The gut is a core regulator of digestion, immunity, and stress response. When it’s in balance, you feel steady and energized. When it’s disrupted, symptoms spread fast.
Next, we’ll break down the most common symptoms of poor gut health and how to recognize early signs before they become chronic.
Poor Gut Health Symptoms
The gut sends signals when it’s struggling. Some signs are mild and annoying. Others are strong warnings. Knowing the difference helps you take the right steps early.

Common Everyday Symptoms
These are the signs most people feel first. They often appear right after meals or during the daily routine.
- Bloating: A heavy, swollen feeling in the stomach.
- Gas: Frequent burping or passing gas throughout the day.
- Constipation: Hard, dry, or infrequent stools.
- Diarrhea: Loose, urgent stools that come suddenly.
- Heartburn or Acid Reflux: Burning sensation in the chest or throat after eating.
- Unpredictable Bowel Movements: Switching between constipation and diarrhea.
- Abdominal Discomfort After Meals: Stomach tightness, pressure, or pain after eating.
These symptoms mean digestion is not running smoothly. They don’t always indicate disease, but they do show that the gut is out of balance.
System-Wide Symptoms Linked to Gut Imbalance
The gut influences more than digestion. When the microbiome gets disrupted, it can affect energy, skin, and mood.
- Chronic Fatigue: Feeling tired even after enough sleep.
- Brain Fog or Difficulty Focusing: Slow thinking or poor concentration.
- Mood Swings / Anxiety-Like Patterns: Stress feels heavier and harder to control.
- Skin Flares: Acne, eczema, rashes, or redness are becoming more frequent.
- Bad Breath: Persistent odor even after brushing.
- Sugar or Junk Food Cravings: Gut bacteria can influence taste and appetite cues.1Do Gut Microbes Taste?, National Institute of Medicine.
These symptoms don’t prove the gut is the root cause every time. But when they appear alongside digestive issues, the link is usually real.
Warning Signs You Should Not Ignore
These symptoms can signal something more serious than a basic gut imbalance. Do not self-treat or wait these out.
- Blood in Stool
- Persistent Diarrhea or Vomiting (more than 48 hours)
- Unexplained or Rapid Weight Loss
- Severe or Sharp Abdominal Pain, Especially at Night
- Fever Combined with Stomach Symptoms
- Family History of Colon Disease, IBD, or Colon Cancer
These signs need medical evaluation, not home remedies. Addressing them early protects long-term gut and overall health.
Key takeaway: Mild symptoms show the gut is struggling. System-wide symptoms show the imbalance is spreading. Red-flag symptoms are the signal to seek medical care.
Next, we’ll look at the real causes behind poor gut health and which ones you can fix naturally.
What Causes Poor Gut Health?
Gut problems don’t appear out of nowhere. They come from daily habits that slowly disrupt digestion and the microbiome. Once you understand the triggers, improving gut health becomes much easier.
Low Fiber and Lack of Plant Diversity
Most people don’t eat enough fiber. Fiber feeds the good bacteria in the gut. When the diet is low in fruits, vegetables, whole grains, legumes, and seeds, the microbiome loses diversity.
What this leads to:
- Slower digestion
- Hard or infrequent stools
- Bloating and gas
- Lower microbial resilience
Simple rule: More plants → more good bacteria → better digestion.
Ultra-Processed Foods and High Sugar Intake
Processed snacks, sugary drinks, packaged meals, and fast food change the microbiome in the wrong direction.
These foods:
- Promote inflammation
- Encourage growth of “harmful” bacteria
- Provide calories but no support for gut repair
Too much sugar also feeds yeast and gas-producing bacteria, leading to bloating and cravings.
Irregular Meal Timing and Eating Too Fast
The gut works best when meals follow a consistent rhythm.
- Eating quickly → poor chewing → digestion overload.
- Skipping meals → acid imbalance and stomach irritation.
- Constant snacking → gut stays in “processing mode” with no time to reset.
Slow eating and regular meals help the gut stay calm.
Chronic Stress
The gut and brain communicate constantly.
Stress changes gut movement and enzyme release.
Stress can:
- Slow digestion → bloating and constipation
- Speed digestion → loose stools and urgency
- Trigger stomach tightness and nausea
Managing stress isn’t “emotional advice.” It’s a biological requirement for gut function.
Poor Sleep
Good gut bacteria follow a day–night rhythm. When sleep is short, inconsistent, or low-quality, microbiome balance shifts.
- Poor sleep → more inflammation → weaker digestion.
Aim for 7–8 hours, not as an ideal, but as normal body maintenance.
Frequent Use of Antibiotics or Antacids
These medications help when needed, but they also:
- Reduce beneficial bacteria
- Change stomach acid levels
- Alter the digestion speed
If used often, they can weaken digestive strength and microbiome stability. Always use them under guidance, not casually.
Smoking, Heavy Drinking, & Excess Artificial Sweeteners
Not demonizing—just stating facts.
- Smoking irritates the gut lining and reduces blood flow.
- Binge drinking inflames the digestive tract.
- Some artificial sweeteners can shift bacterial balance in sensitive individuals.
Moderation is the key here, not perfection.
How These Factors Lead to Symptoms
The chain is simple: Food and habits → change the microbiome → inflammation rises → digestion reacts → symptoms appear.
When the microbiome is balanced, the gut stays stable. When it’s disrupted, even normal foods can trigger discomfort.
How To Fix Gut Health Naturally (Evidence-Based Steps)
You don’t need complicated detoxes or restrictive diets to repair gut health. The gut responds best to consistent, simple habits. Start with these core steps.
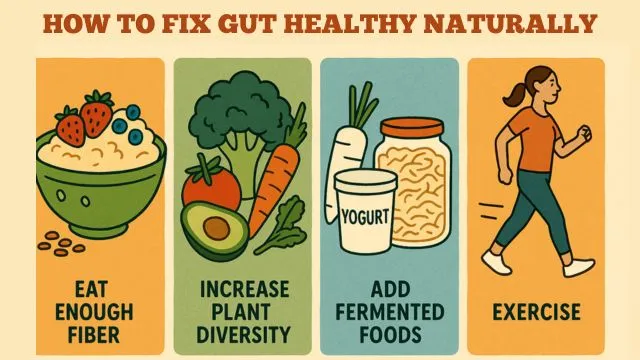
1. Eat Enough Fiber (Most People Don’t)
Fiber feeds the beneficial bacteria in your gut and keeps digestion moving smoothly. Most adults fall far below recommended levels.
- Daily Target: 25–35 grams of fiber per day
- Easy Sources: whole oats, quinoa, beans, berries, chia seeds, sweet potatoes, whole wheat pasta.
Important: Increase fiber slowly to avoid bloating. Give your gut time to adjust.
2. Increase Plant Diversity (Not Just “Eat More Veggies”)
A diverse microbiome is a strong microbiome. Different plant foods feed different bacteria.
- Goal: 25–30 different plant-based foods per week
- Food Items: Vegetables, Fruits, Lentils and beans, Whole grains, Nuts and seeds, Herbs and spices
- Quick Example: Spinach + carrots + tomatoes + onion + garlic + dal + turmeric + rice = 8 plant items in one meal.
Small changes → big diversity boost.
3. Add Fermented Foods (Consistently)
Fermented foods bring beneficial live bacteria into the gut.
- Food Items: Curd / Yogurt (unsweetened), Kefir, Idli / Dosa batter (naturally fermented), Kanji (fermented rice drink), Sauerkraut, & Kimchi
- Key point: You don’t need a large amount. A small serving daily works better than a large serving once in a while.
4. Eat Prebiotic-Rich Foods
Prebiotics are food for good bacteria. They help beneficial microbes grow.
- Prebiotic-Rich Choices are Oats, Garlic, Onions, Bananas (slightly firm, not overly ripe), Lentils and chickpeas, Apples, Asparagus, etc
- Combine prebiotics + fermented foods for a strong gut combo.
5. Hydration Matters More Than People Realize
Water keeps stool soft and easier to pass. Dehydration slows digestion and increases gas.
- Simple Rule: If your urine is pale yellow, hydration is good, and if it’s darker, drink more.
- A common target: 6–8 cups of water per day, more in hot weather or with exercise.
6. Exercise (Not Optional for Gut Health)
Movement improves microbiome diversity and digestion speed.
- Weekly Target: 150–270 minutes of moderate exercise
- Mix in strength training 2–3 times a week
- Even 10-minute walks after meals help reduce bloating and improve gut motility.
7. Sleep & Stress Reset
Your gut and brain communicate constantly. Poor sleep and high stress change bowel habits and appetite signals.
Targets to Aim For:
- 7–8 hours of quality sleep each night
- Daily parasympathetic activities like:
- Deep breathing
- Light stretching
- Slow walks
- Journaling or quiet wind-down time
These calm the nervous system, helping the gut function steadily.
Key Takeaways: Gut healing is not about perfection. It’s about consistent, small improvements; More fiber, more plant variety, steady hydration, and movement. Less stress on the system. These habits restore balance from the inside out.
The 7-Day Gut Reset (Simple, Clear, Actionable)
This plan helps your gut calm down and reset. It focuses on routine, not restriction. Follow it for one week and observe how your digestion feels.
Daily Routine Framework
Morning
- Drink 1–2 glasses of water right after waking up.
- Start breakfast with fiber first (oats, fruit, chia, or whole grains).
Meals
- At least one fermented food per day (curd, yogurt, kefir, or fermented batter foods).
- Pair prebiotics + probiotics:
- Example: Curd + banana, Yogurt + oats, Idli + sambhar.
After Meals
- Take 10-minute slow walks after lunch and dinner to reduce bloating.
Evening
- Keep a 2-hour gap between your last meal and sleep.
- Avoid screens and heavy snacks late at night.
Consistency matters more than perfection.
7-Day Example Meal Plan
Veg Version
- Breakfast: Oats with banana + chia seeds
- Lunch: Dal, brown rice/millets, vegetables, salad
- Snack: Apple or roasted chickpeas
- Dinner: Vegetable khichdi + curd
Non-Veg Version
- Breakfast: Eggs + whole-grain toast + fruit
- Lunch: Grilled chicken/fish + vegetables + rice
- Snack: Nuts or yogurt
- Dinner: Lentil soup + sautéed vegetables + curd
Keep meals simple, warm, and easy to digest.
High-Fiber Grocery List
Add these to your kitchen for the week:
- Oats or daliya
- Lentils (dal), chickpeas, kidney beans
- Brown rice or millets
- Leafy greens and mixed vegetables
- Apples, bananas, guava
- Chia seeds or flaxseeds
- Curd or yogurt (unsweetened)
This list supports digestion, feeds good bacteria, and reduces cravings.
Key Idea: You don’t need drastic diet changes. Regular water, steady fiber, daily fermented foods, and light walking can reset your gut faster than extreme cleanses or supplement stacks.
We have created a detailed, 7-day simple, and actionable gut rest plan, which is totally free. Include this diet routine for better gut health. Download the free PDF below. You can print and paste the plan in your bedroom or kitchen so you remember to follow the easy steps.
30-Day Gut Healing Progress Checklist
Gut healing works best when you track what changes. You don’t need apps or complicated journals. Use this simple checklist daily or every few days to see what’s improving and what needs attention.
1. Stool Form Check
Use the Bristol Stool Scale idea:
| Type | Description | What It Means |
|---|---|---|
| 1–2 | Hard, dry, pebble-like stools | You likely need more fiber + more water |
| 3–4 | Smooth, soft, easy-to-pass stools | Ideal digestion |
| 5–7 | Loose or watery stools | The gut is inflamed or irritated |
- Goal: Aim for Type 3–4 consistently.
- Write one number each day. Takes 2 seconds.
2. Bloating Log
Bloating means gas is getting trapped or digestion is slowed. Rate bloating once per day:
| Rating | Feeling |
|---|---|
| 0 | No bloating at all |
| 1 | Slight fullness that goes away |
| 2 | Noticeable bloating, annoying |
| 3 | Strong bloating affects comfort |
- Goal: Move from 2–3 levels → 0–1 levels by Week 4.
3. Meal Regularity Score
Eat meals in a steady rhythm. Your gut works smoothly when it knows when food arrives. Track yes or no each day:
| Habit | Did you follow it today? |
|---|---|
| Ate meals at regular times | Yes / No |
| Chewed food slowly | Yes / No |
| Did not snack right before bed | Yes / No |
- More Yes days = easier digestion.
4. Sleep Hours Consistency
Poor sleep disrupts the microbiome. Quality sleep helps the gut repair itself at night.
Record how long you slept:
- Less than 6 hours → Gut stress increases
- 7–8 hours → Balanced recovery window
- More than 9 hours regularly → Energy imbalance or fatigue pattern
- Goal: Steady 7–8 hours most nights.
5. Stress Reduction Target
Your gut reacts to stress instantly. Tracking stress helps break the cycle. Each day mark:
| Level | Description |
|---|---|
| Low | Calm, balanced day |
| Medium | Manageable stress |
| High | Stress affected your digestion, mood, or appetite |
Add one daily relaxation habit:
- 5 minutes of deep breathing
- Light evening walk
- Stretching before bed
- Short journaling
- Music without screens
Small consistency beats intense effort.
How to Use This Checklist
Fill it in briefly at night or the next morning:
- Stool type → number
- Bloating → 0–3
- Meal rhythm → yes/no
- Sleep → hours slept
- Stress → low/medium/high
You’ll start noticing patterns:
- Which foods help
- Which meals trigger issues
- Which routines make digestion smooth
Key Takeaway: Healing the gut takes weeks, not days. Tracking helps you see the improvement clearly, even when it feels slow. This system keeps progress visible and motivating, not guesswork.
Our Editorial Summary
Poor gut health comes from everyday habits—low fiber, processed food, stress, irregular meals, poor sleep, and disrupted microbiome balance. The symptoms usually show up first as bloating, gas, constipation, diarrhea, or fatigue. In some cases, the effects spread to mood, skin, and energy levels.
Fixing gut health does not require extreme diets. It requires consistency:
- Eat enough fiber and increase plant diversity.
- Include fermented and prebiotic foods daily.
- Stay hydrated and walk after meals.
- Keep meals regular, sleep 7–8 hours, and manage stress.
- Track progress week to week, not day to day.
Small, repeatable habits restore balance. Not quick fixes. Not detoxes. Just steady input that lets the gut recover and stabilize.
Scientific References
- 1Do Gut Microbes Taste?, National Institute of Medicine.


Recent Posts